At the heart of the Institute of Clinical Bioethics’ commitment to compassionate care and community service are students who go beyond the classroom to make a tangible impact. This blog post highlights the work of Graduate Fellow Shayne Ryan and Undergraduate Research Fellow Ean Hudak in their roles at the wound care clinic. They play a vital role in the operation of the wound care clinic at the Mother of Mercy House in Kensington, Pennsylvania—a clinic that has become a lifeline for individuals facing homelessness, substance use, and chronic wounds. Their collaborative efforts reflect not only clinical dedication but also a deep commitment to the Jesuit values of service, justice, and human dignity.

Shayne Ryan (Master of Business Administration, ’27)
My experience at the wound care clinic has been nothing short of exceptional. Going into this, I was prepared to help underserved individuals, but I wasn’t prepared for how deeply rewarding it would be serving them. What we are doing at the clinic is truly something special. We meet people at some of the lowest points in their lives and not only offer them care, but also dignity and compassion.
As college students, it’s surreal that we can do this work. I don’t know many other people who can say that they are running a fully functional wound care clinic in a city that needs it more than ever. Our team—consisting of Father Clark, EMTs Ean and Emma, as well as Blake and Fredy—ensures the clinic operates efficiently while treating every patient with the highest level of dignity and respect.
The clinic is located in the Mother of Mercy House in Kensington, PA. It consists of a little room which we have transformed into a fully operational clinic that includes an examination table, supply cabinet, scale, workstation, all the wound care supplies, privacy dividers, and a mobile operating light. We couldn’t be more grateful to have such an amazing setup to provide the best care for these individuals. When a patient comes in, we welcome them with open arms no matter their background. They are asked a series of questions to allow a colleague to gather important research data, while Ean, Emma, or I expose and examine the wound. We clean and treat the wound to the best of our abilities, providing the highest level of care possible. Some wounds vary greatly in size and severity, but we always see and treat every patient.
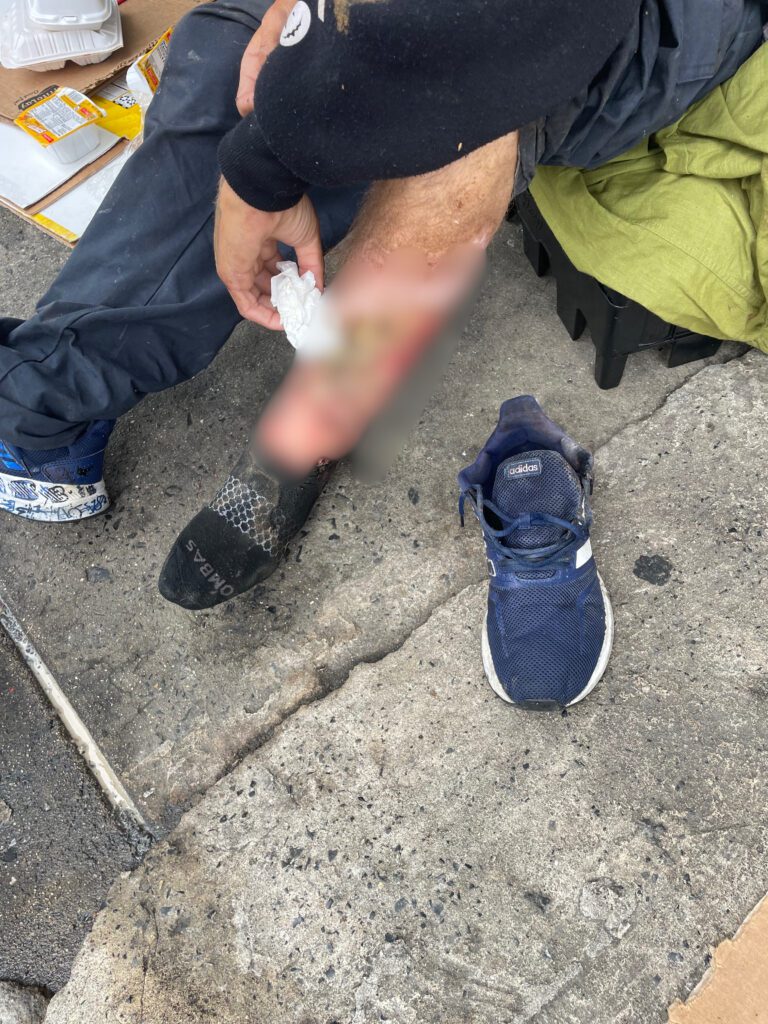
A lot of the wounds we have been seeing in the clinic are caused by a drug called xylazine. Substances like heroin and fentanyl are being laced with xylazine. In the clinic, we have found that individuals who use substances laced with xylazine get wounds on their extremities, usually on their forearms or shins. These wounds can become necrotic if not taken care of properly and can result in amputation. After treating the wounds, we provide each patient with a bag full of wound care supplies, so they can change the bandage themselves when we are not there. We also give them an information sheet listing locations where they can receive free wound care, antibiotics, showers, and meals when the clinic is not open. We are currently working to acquire additional supplies for the clinic, including an automated external defibrillator (AED), a ZOLL monitor for mobile wound care, and a fully stocked trauma bag. These would be a tremendous addition to the clinic, as they will help expand our scope of care.
Ean Hudak (Biomedical Sciences, ’26)
When I began doing wound care back in the Fall of 2024, the room consisted of a few folding tables and chairs to treat patients. Thanks to the support of Mother of Mercy House (MOMH), we now have a fully equipped clinic space with an exam chair, ample cabinet storage, and a well-stocked supply inventory. It was generous of MOMH to allow the wound care team and medical residents to have a voice in building the clinic and designing a space that would suit us best. Before we established the clinic, wound care at MOMH was limited to just two hours on Thursdays. In April, we began exploring ways to improve access and discovered that, under Pennsylvania EMS protocol, EMTs are authorized to provide wound care. In collaboration with Diane and Karl from MOMH, we scheduled wound care on Mondays, as they offer an Olive Garden lunch to the entire neighborhood, including those experiencing homelessness. This not only provides people with a fresh, hot meal, but also creates opportunities for meaningful conversations, allowing us to learn about their hardships and assess whether they need treatment—ultimately allowing us to reach and care for more patients on those days.
Every day in Kensington is something different. Some days are calm with only a few patients, while others are hectic, with back-to-back cases and people waiting. On particularly intense days, we find ourselves rushing across the street to provide basic life support before paramedics arrive. We have administered Narcan to two individuals experiencing respiratory failure, both of whom responded positively. One man was having a drug-induced seizure, forcing us to only give him Narcan while maintaining a patent airway. Thankfully, on all occasions paramedics arrived promptly and administered medications, transporting patients to the hospital for further treatment. Every patient we encounter offers an invaluable experience that will stay with us as we grow into future healthcare providers. We strive to make our patients feel seen and heard by providing patient-centered care grounded in dignity and respect.
Thanks to our outstanding team, we’ve treated just over 50 patients since May. We have drastically increased the quality of our data collection through our ongoing efforts to provide our community and colleagues with information regarding drug-related wounds in Philadelphia. In addition, the patient form has been updated to include new data points—ethnicity, country of origin, housing status, and drug of choice—offering us a more comprehensive understanding of each individual’s background.
Sometimes during treatment, there are a few who are under the influence, and in response, we’ve implemented medical bands that remind patients to follow up with clinics, including ours, and it has the date of treatment included so other places know when they were last treated. The past few weeks, we strengthened our connection with Project HOME which allows patients access to housing, medical treatment, and additional services while providing continuity of care. We are working with Temple’s Podiatry School to implement students in wound care, so they can provide more detailed information about lower extremity wounds and their impact on the patient’s health. It takes one patient’s needs to make a world of difference for others and that begins with a conversation. Moving forward, we will continue to embody Jesuit values and pursue innovation, as these principles lie at the heart of the ICB’s mission.

Example of a necrotizing wound caused by xylazine exposure.